
By Banish & Sylvia Harnarain
For anyone who has struggled with acne, the feeling of finding a treatment that finally works is pure relief. You follow the routine, you see the results, and you think, "This is it. I'm finally done." But what happens when that one holy grail acne treatment suddenly stops working?
This is a common, frustrating experience, especially with popular prescription combinations like Clindamycin Phosphate and Benzoyl Peroxide gel. If you've found yourself searching for answers to why your skin relapsed, you're not alone.
When Clindamycin and Benzoyl Peroxide Work Wonders
Many people experience initial, dramatic success with a combination treatment of Clindamycin Phosphate and Benzoyl Peroxide (often referred to as BPO).
- Clindamycin Phosphate is a topical antibiotic. Its job is to kill Cutibacterium acnes (C. acnes), the bacteria that live on the skin and contribute to acne by causing inflammation.
- Benzoyl Peroxide (BPO) is a powerful ingredient that works in two ways: it kills C. acnes bacteria and helps unclog pores.
When used together, this duo is highly effective. The antibiotic tackles the bacteria, and the BPO helps clear the skin and, crucially, helps the antibiotic work better. For a time, the skin clears up, the inflammation subsides, and life feels normal again.
Why is Clindamycin Phosphate Not Working Anymore? The Science of Resistance
The most significant reason why your once-effective treatment may fail is antibiotic resistance.
When you use a topical antibiotic like clindamycin for an extended period, the C. acnes bacteria on your skin can evolve and become resistant to the drug. This means the antibiotic can no longer kill the bacteria, and your acne returns.
Dermatologists are now highly cautious about prescribing topical antibiotics alone. The scientific consensus is clear: topical clindamycin should always be combined with Benzoyl Peroxide to minimize the risk of resistance [1].
The Role of Benzoyl Peroxide in Fighting Resistance
Benzoyl Peroxide is a potent antibacterial agent that works differently from antibiotics. It releases oxygen into the pore, which is toxic to the C. acnes bacteria (which are anaerobic, meaning they hate oxygen). Bacteria cannot develop resistance to Benzoyl Peroxide [2].
So, if you were using the combination, why is Clindamycin Phosphate not working?
- Resistance Emerged Anyway: While BPO significantly reduces the risk, resistance can still emerge over time, especially if the treatment is used for many months or years.
- The BPO Concentration Was Too Low: The BPO component may not have been strong enough or used consistently enough to suppress the resistant bacteria fully.
- Underlying Acne Factors: Your acne may be driven more by hormones, genetics, or inflammation than by bacteria alone. Once the antibiotic is ineffective, these other factors take over.
Why is Benzoyl Peroxide Not Working? It's Not the Whole Story
If you are still using a BPO product and your acne is back, you might be asking, "Why is Benzoyl Peroxide not working?"
The truth is, BPO is still working as an antibacterial, but it can't solve all your acne problems on its own. Acne is a complex disease with four main contributing factors:
| Factor | Description | How BPO Helps |
|---|---|---|
| 1. Excess Sebum (Oil) | Overproduction of oil by the sebaceous glands. | Indirectly, by reducing inflammation. |
| 2. C. acnes Bacteria | Proliferation of acne-causing bacteria. | Directly kills bacteria by releasing oxygen. |
| 3. Inflammation | Redness, swelling, and pus formation. | Reduces inflammation by controlling bacteria. |
| 4. Follicular Hyperkeratinization | Dead skin cells clogging the pore opening. | Helps unclog pores (mildly keratolytic). |
BPO is excellent at tackling the bacterial factor, but it is less effective at treating the root cause of the clogged pores (hyperkeratinization) or the hormonal drivers of excess oil.
Try Other Acne Treatments Like Retinol
The latest dermatological guidelines emphasize the use of topical retinoids (like Tretinoin, Adapalene, or Tazarotene) as an acne treatment [3]. Retinoids are Vitamin A derivatives that directly target the clogged pore factor (hyperkeratinization) and reduce inflammation.
If your acne has relapsed, your dermatologist will likely pivot to a regimen that includes a retinoid, that may be in combination with benzoyl peroxide, to address the problem from multiple angles.
Beyond Topicals: The Impact of Stress, Diet, and Hormones
Sometimes your body just needs some extra support and care. You can try "eating clean" as that tends to help my acne and an acne flare tends to happen for me during stressful periods of poor sleep and honestly my diet is filled with more snacks and processed foods when I'm stressed too.
Scientific research increasingly supports the link between these factors and acne severity:
- Stress: High stress levels increase the production of hormones called androgens and corticotropin-releasing hormone (CRH), which can stimulate oil glands and trigger inflammation, leading to breakouts [4].
- Diet: While the link is complex, high-glycemic index foods (like white bread and sugary drinks) and dairy products have been shown in some studies to exacerbate acne in susceptible individuals [5].
When your body is under stress, even the best topical treatments can be overwhelmed by internal hormonal and inflammatory signals.
Exploring Alternatives: The Role of MSM and Natural Ingredients
The frustration of failed prescription treatments often leads people to explore natural alternatives. One ingredient gaining attention in the natural skincare space is Methylsulfonylmethane (MSM).
MSM is an organic sulfur compound known for its anti-inflammatory properties. While research is still emerging, studies suggest that MSM may help improve skin health by:
- Reducing Inflammation: MSM can help calm the redness and swelling associated with inflammatory acne [6].
- Strengthening Skin: It is a source of sulfur, a key component of keratin, which is vital for healthy skin structure.
For those looking to transition to a more natural approach after experiencing antibiotics like Clindamycin Phosphate not working, products that leverage ingredients like MSM can be a gentle, supportive step.
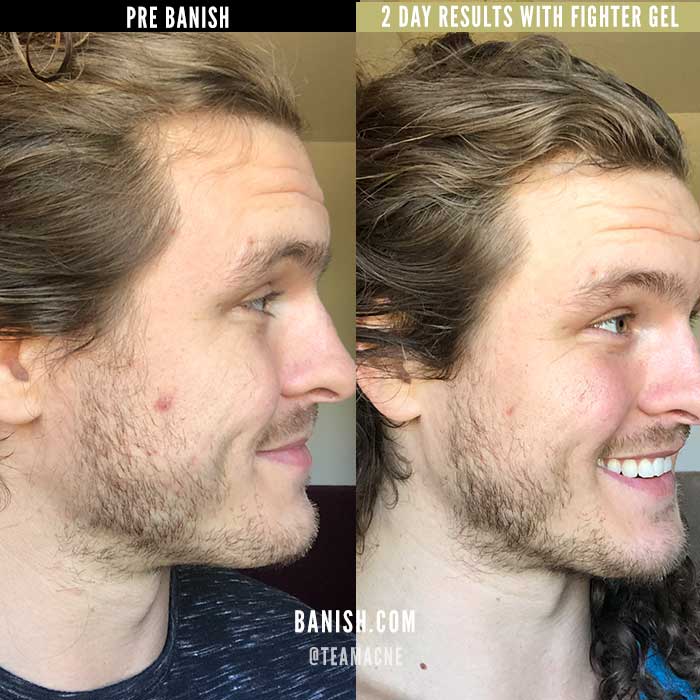
For example, the Banish Fighter Gel is formulated with MSM, along with other soothing ingredients like Aloe Vera and Centella Asiatica, to help calm breakouts and reduce redness without the harshness of traditional acne medications.
What to Do When Nothing is Working
If you are experiencing the frustration of having your acne treatment fail, here are the next steps recommended by dermatologists:
- Stop Using Topical Antibiotics Alone: If you are using clindamycin or erythromycin without BPO or a retinoid, stop and consult your doctor.
- Consider Systemic Treatment: For severe, cystic, or relapsing acne, systemic treatments like hormonal therapies (for women), or Isotretinoin (Accutane) may be something to consider - but be knowledgeable about the side effects too.
- Address Lifestyle: Manage stress, prioritize sleep, and consider an anti-inflammatory diet.
The journey to clear skin is rarely a straight line. By understanding the science behind why clindamycin phosphate not working is a common issue—namely, antibiotic resistance—you can work with your doctor to find a more sustainable, multi-faceted treatment plan.
References
[1] Efficacy and safety of clindamycin phosphate 1.2%/tretinoin 0.025% formulation for the treatment of acne vulgaris: pooled analysis of data from three randomised... European Journal of Dermatology. (2014). https://www.sciencedirect.com/science/article/pii/S0190962215026146]
[2] The role of benzoyl peroxide in the new treatment paradigm for acne. Journal of Drugs in Dermatology. (2013). https://pubmed.ncbi.nlm.nih.gov/23839205/]
[3] Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology. (2016). https://www.jaad.org/article/S0190-9622%2815%2902614-6/fulltext]
[4] The effect of stress on skin barrier function and its relationship to inflammatory skin diseases: a review. Journal of the European Academy of Dermatology and Venereology. (2014). https://onlinelibrary.wiley.com/doi/10.1111/ijd.15390]
[5] Diet and acne: a review of the evidence from 2009 to 2020. International Journal of Dermatology. (2021). https://onlinelibrary.wiley.com/doi/10.1111/ijd.15390]



















Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.