- What's fungal acne
- Other Skin Conditions Related to Fungal Acne
- What Causes Fungal Acne?
- How to Tell If You Have Fungal Acne
- How to Treat Fungal Acne
- What to Avoid
- Foods That May Worsen Fungal Acne
- Products for Fungal Acne
- Can I Prevent Fungal Acne?
- My Experience
- Conclusion
What Is Fungal Acne?
- Size: Fungal acne typically consists of uniform, small pus-filled bumps, while bacterial acne varies in size.
- Location: Fungal acne commonly appears on the chest, back, and upper arms, while bacterial acne is more prevalent on the face.
- Itching: Fungal acne causes significant itchiness, unlike bacterial acne.
- Clusters: Fungal acne often appears in clusters, resembling a rash, while bacterial acne is more spread out.
It can look like a cluster of whiteheads that are usually on the t-zone since it feeds off of sebum.
A fungal acne is a type of infection found in your skin’s hair follicles that commonly appears as small whiteheads. It is often left with persistent bumps that do not go away with conventional acne treatments targeted toward reducing bacterial acne.
Fungal acne doesn't vary much in shape or size. Fungal acne can actually coexist in people with acne at a rate of 12-17% so it's possible to have both acne and Malassezia at the same time.
If you have these skin conditions, it's likely you may have fungal acne too.
- Eczema
- Dandruff
- Seborrheic Dermatitis
- Psoriasis
Here's how to tell if you have fungal acne and the common ways to treat it.
These skin conditions are related to Malassezia. They include eczema, dandruff, seborrheic dermatitis, and Psoriasis. As mentioned before, type of fungal skin infection will not respond to traditional medications for bacteria acne such as topical antibiotics, and benzoyl peroxide. It is actually advised against to take any kind of antibiotics because both bacteria and fungi exist together to utilize the same resources from our body. If there are not enough bacteria to compete with the fungi, the fungi will outgrow the bacteria, causing a yeast infection.
If you suspect that you might be suffering from fungal acne, it is recommended to get it checked out by a dermatologist to confirm it.
What Causes Fungal Acne?
- Overgrowth of Yeast: An imbalance in your skin’s microbiome, often due to antibiotic use, can lead to fungal acne.
- Trapped Moisture: Wearing sweaty or tight clothing traps moisture and oil, creating the perfect environment for yeast to grow.
- Medications: Antibiotics can disrupt the balance of bacteria and fungi, allowing yeast to proliferate.
- Weakened Immune System: A suppressed immune system makes you more susceptible to fungal infections.
- Diet: Diets high in refined carbohydrates and sugar can feed yeast growth.
- Hot and Humid Climates: Warm weather and sweating can exacerbate fungal acne
How To Tell If You Have Fungal Acne
Usually fungal acne doesn't respond to benzoyl peroxide or antibiotics.
SYMPTOMS OF FUNGAL ACNE
So, how do we know or determine if our acne is a fungal type of acne or not? One big different to tell if your acne is fungal, is if it gets frequently itchy unlike acne.
1. Size - Fungal acne tends to appear like small pus-filled bumps and tend to be nearly the same size throughout.
2. Location - Fungal acne doesn't appear as often on the face, and more often on the arms, chest and back.
3. Itching - Another difference between fungal acne and bacterial acne would be the itchiness. Fungal acne causes itchiness while bacterial acne does not.
4. Clusters - You would know that your acne is a fungal type if it often appears in clusters of small whiteheads.
How To Treat Fungal Acne
Treating fungal acne is not the same as treating regular acne – fungal acne won't respond to some acne treatments.
Below are a list of common fungal acne treatments. Remember to always patch test these products on a small area of your skin so you know will know if any ingredients are irritating your skin before you put it all over your face and body. Otherwise, you may be making your skin worse without even realizing it and although you have treated your fungal infection, now you would have a new problem dealing with break outs from an ingredient your skin is allergic or sensitive to.
HOW TO TREAT FUNGAL ACNE
Fungal Acne needs to be treated with antifungals, with avoidance of antibiotics and antibacterial cleansers. Eliminate topicals that contain oils so look for oil free products, and try to shower or change out of your clothes as soon as you can if you've sweated.
Anti Dandruff shampoos - Dandruff shampoos may be recommended such as Nizoral or Selsun, with the main active ingredient zinc pyrithione. Anti dandruff shampoos should be in contact with the part of the body that needs to be treated for 5 minutes before rinsing.
Athlete's foot cream - An over the counter athelete's foot cream can also be used for some types of fungal acne, and the main anti-fungal ingredient is called clotrimazole.
Anti Fungal Prescriptions: If over the counter methods aren't working, you can see a professional for a prescription. There are at least 2 prescribed medications for treating fungal acne: Fluconazole and Ketoconazole.
Fungal Acne Home Remedies
If you want to try home remedies instead Here are home remedies that would aid in keeping those fungal acne at bay:
- Lactobacillus
- Honey
- Tea tree oil
- Apple cider vinegar
Lactobacillus – This home remedy produces lactic acid that could control yeast production. Taking lactobacillus supplements may help with reducing fungal overgrowth.
Honey – Honey is known for its antimicrobial properties, making it one of the recommended home remedies for treating fungal acne and studies show it's effective against a form of fungal acne. Use Manuka Honey for this and leave on for 3 hours.
Tea tree oil – Tea tree oil also contains antimicrobial properties like honey and it also has anti fungal properties. Dilute it first in water before applying it to areas with fungal acne.
Sulfur - Sulfur can reduce Malassezia on the skin and sulfur is good at absorbing and reducing skin oils. Look for skincare products that contain sulfur and are oil free.
Apple cider vinegar – May work as treatment due to its antifungal properties and pH balancing properties as some people with eczema may have a high skin pH. You can mix 2 tablespoons of ACV in 2 cups of water and dab the mixture as a toner on affected areas.
What To Avoid
If you realize that you do have fungal acne, it is important to avoid creating a moist environment on your skin as fungus thrives in moist environments. You can still apply hydration on your skin, but avoid occlusives.
It is also important to avoid products with ferments as it may trigger the growth of more yeast. The last thing to avoid is products with long fatty acid chains such as oils, since Malassezia feeds on them, especially in areas on your face where you are the oiliest with the most sebum production.
Foods That May Worsen Fungal Acne
Fungal acne may thrive with sugar, so reducing refined carbs and sugar intake may help improve fungal acne along with the topical changes and using products that are oil free and fungal acne safe.
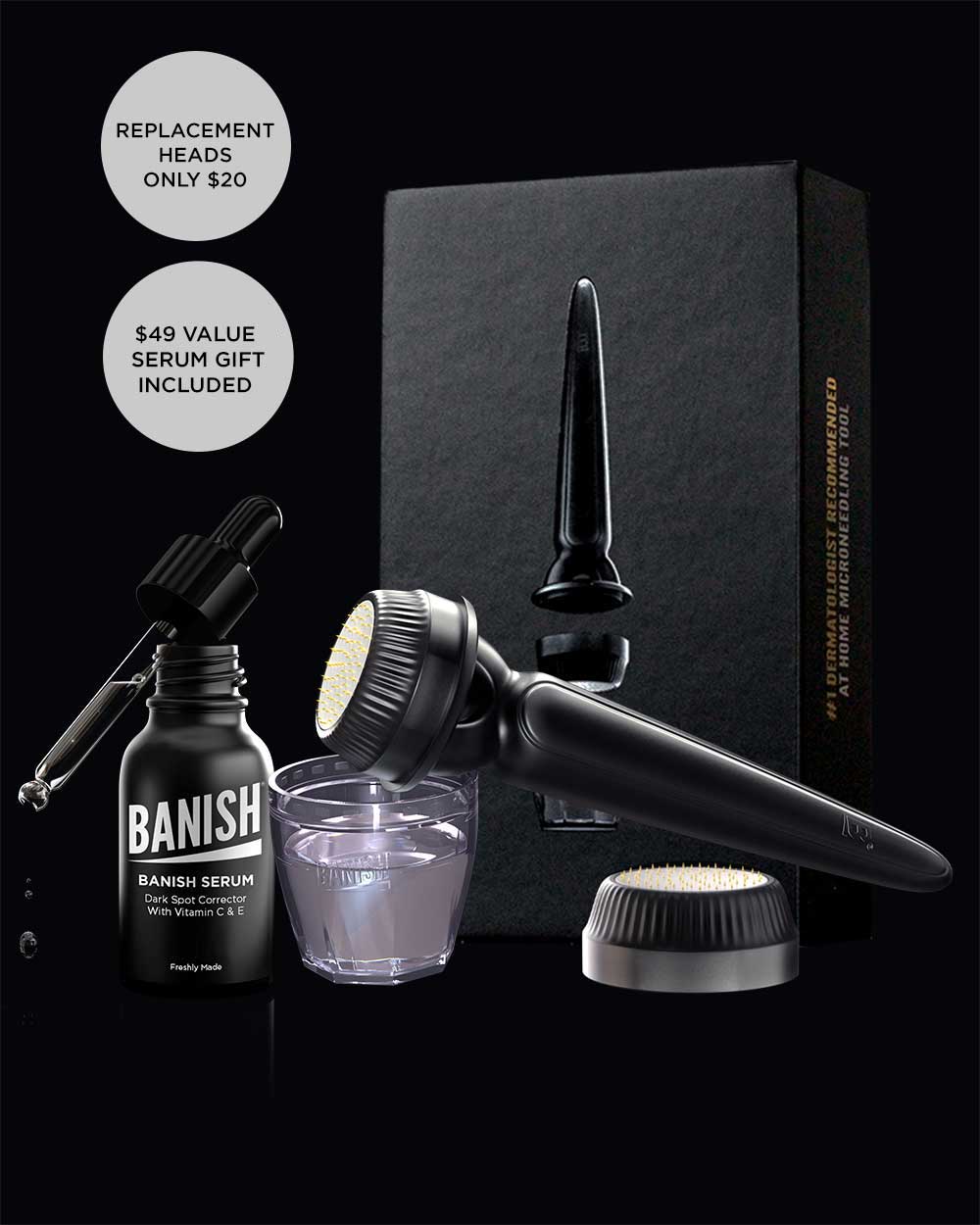
Does Banish Have Fungal Acne Safe Products?
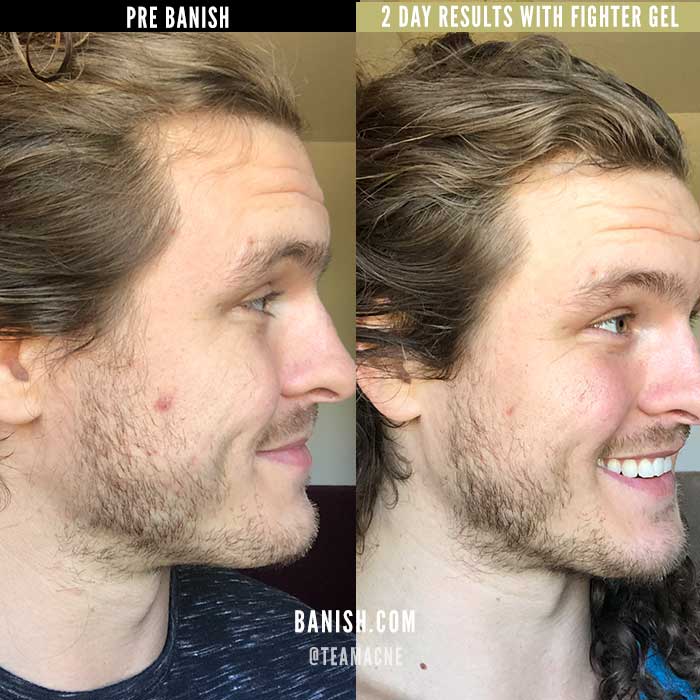
Yes, the skincare we have that's safe to use with fungal acne is the Fighter Gel - as it is water based without fungal promoting ingredients, and it also contains several ingredients with anti-fungal properties such as peppermint oil.
All Clear Mint Cleanser is also fungal acne safe as it doesn't contain any fatty oils.
The Pumpkin Enzyme Masque may also be generally safe to use if you have fungal acne. As a disclaimer, it does contains some oils which can be a potential fungal acne trigger. Note that this is a wash off product after leaving it on for 10 minutes. It also exfoliates the skin.
Glycolic acid sloths off the top layer of skin and also reaches into small pores to break down excess dirt, sebum and oils which can be beneficial for clearing up fungal acne, just remove and wash off with a fungal acne safe cleanser afterwards!
CAN I PREVENT FUNGAL ACNE?
Fungal acne unfortunately can reoccur and can take months of persistent treatment to really manage it. However, there are ways to help keep fungal acne or Malassezia folliculitis at bay by simply following these do’s & don’ts.
Do’s
- Keep skin dry and clean during and after workout session
- Use an anti-fungal body wash at least once a week
- Use products containing salicylic acid or glycolic acids
- Cycle in anti-fungal shampoos to prevent development of fungal acne
- Shower twice a day during hot humid days
Don'ts
- Wear tight clothing (e.g. synthetic fabrics) that traps the sweat
- Re-wear sweaty clothes
- Using products that contain benzoyl peroxide, oils, fatty acids, linoleic acid
MY EXPERIENCE
I’ve recently self-diagnosed myself with fungal acne as I have never had small red closed comedones all over my forehead despite not having many changes in skin care, diet, and lifestyle. I began learning about the causes and discovered fungal acne. Then I started using over the counter anti-fungal products to see if they made a difference and my bumpy skin returned to normal after only a few weeks. I am still continuing with the ketoconazole shampoo and the occasional clotrimazole cream to try to completely eradicate the fungal infection before I add more products into my skincare routine.
CONCLUSION
Differentiating fungal acne from regular acne can be quite tricky so it's best to check with a dermatologist if you can. Delaying with the proper treatment could cause fungal acne or acne to worsen.
Fungal acne requires different treatment protocols and does not respond to typical acne treatment. We hope that this guide has helped you learn more about fungal acne and how to manage it.






















1 comment
Dana Joiner
Very informative article
Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.